How to improve your gut health diet and make it better?
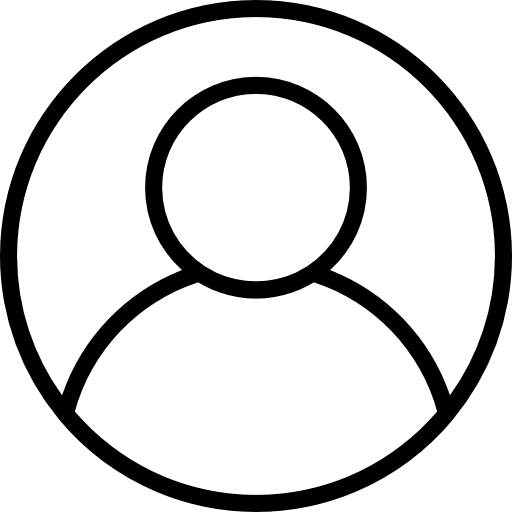
Well, the human body is a rather unusual and amazing place because it is a home to a complex invisible world of living microorganisms that together, with the host, keep our species advanced and healthy by participating in a number of complex metabolic, trophic and defence functions.
It is the organ through which all the complexity of the interaction of the host and the complete community of microorganisms (microbiotas) in the harvest of nutrients and defence against potentially dangerous pathogenic bad bacteria and toxins from food is manifested.
In order to understand at least the most important interrelationships and the way of functioning we have to descend to the level of direct collision, the place of occurrence of interactions, and that is the intestinal mucosa.
It is a kind of boundary between the inner world (organism) and the outer world (intestinal lumen) that is divided by a simple layer of epithelium.
It is in this layer that the body’s first line of defence is called mucous immunity, which consists of intestinal lymphocytes, macrophages, plasma dendritic cells, HBD human beta-defensins, LPMC mononuclear cells, lamina propria, SIgA secretory IgA immunoglobulins that activate to respond.
That is why this place is called MALT (mucosa-associated lymphoid tissue).
The situation is known if we consider that the intestine is the least sterile region of the body because it contains trillions and trillions of mostly bacteria that together, with food intake, make up a significant amount of antigene material that must be well tolerated to tolerate the status quo or homeostasis.
This is precisely the specificity of such an immune defence system in a specific environment called GALT (gut-associated lymphoid tissue).
Unlike its compatriot systemic immune system, which tends to react for a few seconds with a violent reaction to an external antigen, GALT does so by quietly tolerantly eliminating dangerous bacteria, allowing beneficial and less dangerous bacteria to coexist in the outside world without raising a destructive immune system.
Despite the activation of inflammatory cells (lymphocytes and macrophages) with the arrival of bacteria in the LP (lamina propria) of the intestine, there is no development of inflammatory aggressive lymphocytes and macrophages that would create a sick and life-threatening condition.
There is another phenomenon in the form of the appearance of mucosal immunity-resistance to harmful environmental influences, and that is the concept of oral tolerance-tolerance, which implies antigen-specific lack of response to antigen taken orally.
It must be noted that approximately 2% of protein from food avoids complete digestion-degradation and is directly drained into the blood unchanged due to the lack of response-oral intolerance.
The ability of intestinal epithelial cells to distinguish dangerous from less dangerous bacteria or even beneficial ones, and to create a different immune response to each antigen is an extremely complex process that is still being studied in animal and human models.
Best diet for gut health
The intestinal microbiota is strongly associated with daily food consumption, so its composition can serve as a biomarker of nutritional habits, but also the risk of disease associated with these habits.
In certain circumstances, illness, inflammatory bowel disease IBD or colorectal cancer CRC become a "bad guy" – a bad guy of E. coli strain that sticks to intestinal epithelial cells, penetrates, and not only causes inflammation but also feeds on harmful products of that inflammation and creates colibactin genotoxin which destroys DNA and promotes cancer growth.
In order to maintain the balance at the level of microbes-immunity-metabolism, the energy obtained by the host through dietary habits and in conjunction with the microbiota from plant fibres creates energy and protective molecules SCFA (short-chain fatty acids) that drive epithelial cells in the intestine.
Oral tolerance is age-dependent and therefore more difficult for the newborn to achieve due to the more permeable intestinal barrier, immaturity of mucosal immunity-defence and inability to achieve an antibody-dependent response to various food antigens.
Compensation for this condition is the limited supply of food for the newborn that protects it from a strong defensive response to various antigens. After 2 years the microbiota in newborns becomes similar to that in adults.
Giving probiotics to the mother in the period before childbirth and during lactation protects the offspring from the occurrence of atopic eczema, which is a positive effect of Lactobacillus GG on oral tolerance.
In other words, when our microbiota is in balance with our immune system (controlled supported inflammation) we have the best chance of staying healthy. The influence of diet and eating habits on metabolism is known and proven by many authors.
Gut health diet plan
Subjects who were on a high-protein, the low-carbohydrate diet of only 4% of the total meal significantly reduced the level of phenolic excretion of components found in the cell wall of plant fibres that have anti-inflammatory activity, and significantly increased the near-risk level of acetylphenolic acid in rectal water that has procarcinogenic action.
By the action of anaerobic bacteria in the large intestine, plant fibres are subjected to fermentation in SCFA (butyrates, acetates and propionates).
There is a significant association between SCFA levels and the composition of the microbiota with a high concentration in the intestinal lumen with a consequent change in pH level stopping growth anaerobic gram-negative Enterobacteriaceae including pathogenic-bad bacteria Salmonella spp.
The use of antibiotics has a strong effect on microbial intestinal metabolism and consequently on humans. Understanding the process underlying this mechanism remains one of the major goals of research efforts.
The minimum diversity and richness in the total microbial fraction were 11 days, while a collapse of the imbalance of active bacteria was observed 14 days after antibiotic administration.
The greatest metabolic changes of bacteria occurred on day 6 when intestinal bacteria responded to the use of antibiotics by reducing-suppressing the complete energy metabolic state and capacity for transport and metabolism of biliary acids, cholesterol, hormones and vitamins.
Already in 1988. before the first PPI (proton pump inhibitor) was introduced during only 2 weeks of testing omeprazole was shown to increase the number of bacteria in gastric juice.
It has been proven that PPI (omeprazole, pantoprazole…) by breaking the stomach acid barrier allow colonization of the stomach by bacteria from the mouth and environment and their transfer to the small and large intestine causing dysbiosis-disrupted bacterial composition and bacterial overgrowth (SIBO).
There are many other connections between PPI intake and certain infections of the digestive tract with (Clostridium dif., Campylobacter j. Salmonella), impaired absorption of certain nutrients important for normal body function (Fe, B12, Ca) and diseases that have not yet been proven causally.
Scientific research has shown that support with adequate nutrition is as important as medication.
Diet for good gut health
It is extremely important to drink plenty of fluids because of diarrhoea. It is necessary to drink water, teas, non-carbonated juices, but the best one is apple juice.
Compounds are very important, especially for children in the phase of intensive growth. Diarrhoea leads to a deficit (fall) of protein and patients need higher amounts of protein compared to a healthy population.
One scientific study has shown that soy protein is acceptable as a replacement for milk protein in people who are intolerant to milk protein.
Chicken is also a suitable type of meat for the sick.
Fruits, vegetables and grains (if you do not suffer from celiac disease – a disease of intolerance to gluten, which is the main ingredient of all grains), should make up half the calories that patients should take in during the day.
Fresh fruits (apples, grapefruit, plums, raspberries and currants) are considered a protective (good) fruit for patients and the prevention of colon cancer. Patients should avoid fruits with a higher sugar content such as grapes, pineapple, watermelon, pears.
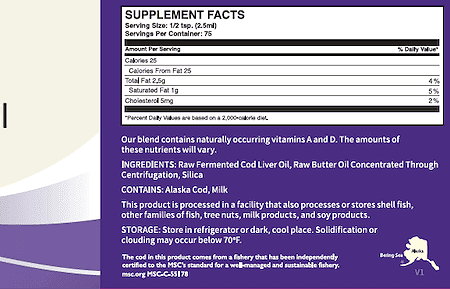
Fish oil, ie blue fish rich in omega 3 fatty acids, is considered to be extremely good for the intestinal mucosa and reduce inflammation of the particularly small intestine.
They are needed in all types of diarrhoea, especially those with chronic intestinal diseases. Almost regularly, such patients lack the element potassium, which is found in foods in fresh cow’s cheese, fish, avocados and bananas.
Fats exacerbate inflammation of the small intestinal mucosa in Crohn’s disease and ulcerative colitis. Patients with chronic inflammatory bowel disease should shed fat, especially saturated fat in meat and dairy products.
However, as mentioned earlier, the fats found in fish oil (omega 3 fatty acids) may help heal inflamed mucous membranes. Some patients with chronic inflammatory bowel disease have lactose intolerance, ie. sugar found in milk.
In these patients, diarrhoea is usually aggravated by drinking milk, but the use of yoghurt (not fruit yoghurt), but plain or with the addition of cultures such as acidophilus and other dairy cultures where milk is fermented, may help reduce inflammation of the intestinal mucosa.
These products should be avoided and not taken when you suffer from chronic intestinal diseases.
Sucrose substitute, is a daily consumable sugar, you can replace some of the simple sugars (monosaccharides) and these are fruit sugar-fructose, dextrose or grape sugar in grocery stores with a delicatessen department) or in pharmacies.
Soy, eggs, tomatoes and peanuts should not be consumed.
Although it was mentioned that patients need potassium, and tomatoes are a food that has a high proportion of them, patients should take a banana, fresh cow’s cheese without cream and fish to compensate for potassium from food, and not tomatoes.
Foods composed of wheat grains, oats, barley, or foods that contain gluten due to the large number of patients who have worsening symptoms due to intolerance (intolerance) of these foods should be eliminated from daily use.
Now, it will be easier to follow your gut health diet while knowing all things mentioned in the article.